Tympanoplasty is a surgical procedure used to repair a perforated eardrum or parts of the middle ear, often needed to treat hearing loss or recurring ear infections. It may also involve replacing damaged ossicles and may be used to treat conditions such as otosclerosis or adhesive otitis media. How is the surgery performed, who can benefit from it, and what to expect during recovery?

What Is Tympanoplasty and When Is It Performed?
Tympanoplasty is a surgery to fix a damaged eardrum or the small bones in the middle ear, known as ossicles, which transmit sound to the inner ear. A hole in the eardrum or damaged ossicles can cause hearing loss or recurring infections. Surgeons perform tympanoplasty to patch the eardrum or rebuild the bones, aiming to improve hearing and prevent infections. Otolaryngologists, or ENT specialists, carry out the procedure using precise tools like microscopes.
Doctors don’t recommend tympanoplasty immediately. They often try simpler treatments, such as ear drops or antibiotics, first. If these fail after a few months, tympanoplasty becomes an option. Surgeons customize the procedure based on the specific ear damage. The goal is to restore hearing and maintain ear health.
Why Hearing Is Crucial
Hearing connects people to conversations, music, and their surroundings. A perforated eardrum can muffle sounds or cause persistent ringing. Tympanoplasty seeks to restore clear hearing. Research shows patients often feel isolated when hearing fades, making this surgery impactful beyond physical repair. It improves daily life by reconnecting individuals to their world.
Who Performs the Surgery?
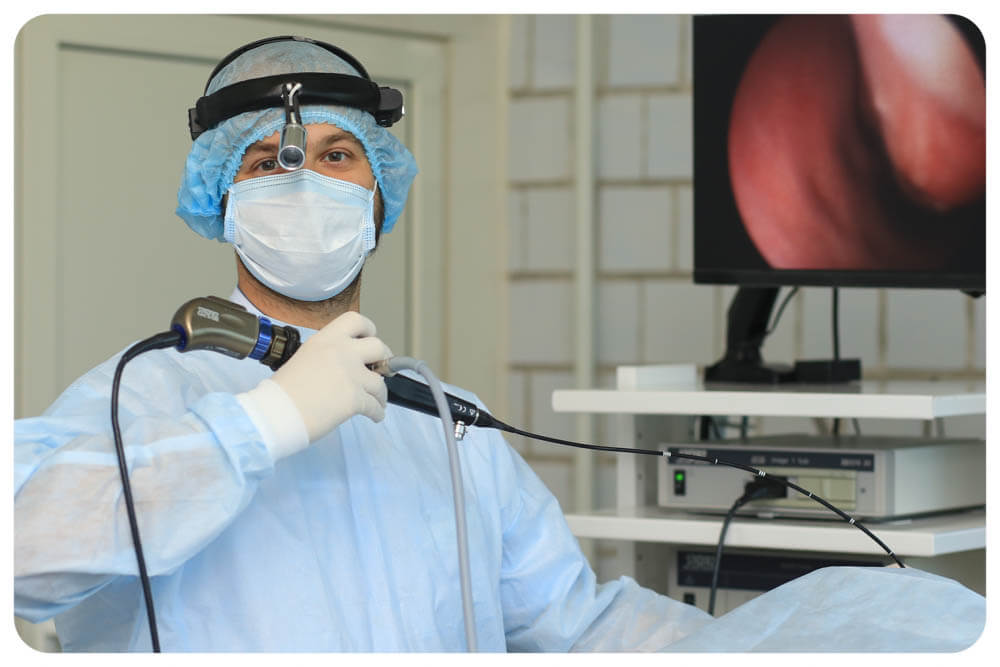
Otolaryngologists, specialists in ear, nose, and throat conditions, perform tympanoplasty. They use advanced tools like microscopes or endoscopes to navigate the ear’s tiny structures. Medical sources highlight their extensive training in delicate procedures like middle ear surgery. Patients can trust these experts to handle the intricate work of ear reconstruction with precision.
Indications for Tympanoplasty
A person may need tympanoplasty if their eardrum has a hole that won’t heal naturally. This can result from infections, injuries, or other ear conditions. Doctors typically wait a few months to see if the eardrum repairs itself. If it doesn’t, surgery is considered. Tympanoplasty also addresses issues affecting the ossicles or causing chronic ear problems.
Common reasons for tympanoplasty include:
- Persistent ear infections that return frequently.
- A perforated eardrum caused by trauma, such as a loud explosion or ear injury.
- Otosclerosis, where the stapes bone becomes fixed, impairing hearing.
- Adhesive otitis, when scar tissue binds the eardrum to the middle ear.
- Cholesteatoma, a skin growth in the middle ear that damages structures.
These issues can lead to hearing loss or constant ear drainage, known as otorrhea. Medical sources note that untreated conditions may worsen, potentially causing dizziness or severe infections. Tympanoplasty is recommended when non-surgical treatments fail to resolve these problems.
Chronic Infections and Their Effects
Chronic ear infections often prompt tympanoplasty. They can erode the eardrum over time, creating a hole that allows bacteria to enter. This triggers more infections, forming a cycle. Patient stories online describe the frustration of ongoing ear pain and discharge. Surgery interrupts this cycle by sealing the hole and strengthening the ear’s defenses.
Trauma and Sudden Damage
Sudden injuries, like a cotton swab mishap or a loud blast, can tear the eardrum. While small tears often heal naturally, larger ones may not. Research indicates about 80% of acute perforations close on their own. If they persist, tympanoplasty prevents long-term hearing issues or infections, acting like a patch to restore function.

Main Steps of the Procedure
Tympanoplasty is a precise surgery, typically performed under general anesthesia in a hospital. The surgeon begins by examining the eardrum with a microscope or endoscope. They access the damaged area through the ear canal or a small incision behind the ear. A graft, essentially a patch, is used to repair the eardrum hole. This graft may come from the patient’s tissue, such as cartilage or muscle lining, or synthetic materials.
Here’s an overview of the steps in tympanoplasty:
| Step | Description | Purpose |
| Preparation | The patient is anesthetized; the ear is cleaned and inspected. | Ensures safety and a clear view of the eardrum. |
| Access | The surgeon enters through the ear canal or makes a cut behind the ear. | Provides access to the damaged eardrum or ossicles. |
| Graft Harvest | Tissue is taken from the patient’s ear or a synthetic material is used. | Supplies material to close the hole. |
| Patching | The graft is placed over the hole and secured with dissolvable packing. | Seals the perforation and supports healing. |
| Closure | Any incision is stitched; the ear canal is packed with cotton. | Protects the repair and aids recovery. |
The procedure can last 30 minutes for simple repairs or several hours for complex ossicle reconstruction. Medical sources explain that the approach depends on the damage’s severity. The ear is packed afterward to stabilize the repair during healing.
Types of Grafts Used
The graft is central to eardrum repair. Surgeons may use the patient’s temporalis fascia, a tissue near the temple, due to its similarity to the eardrum. Cartilage from the ear or fat from the earlobe are other options. Synthetic materials, like gel foam, suit smaller holes. Studies report success rates around 90% for most grafts, with each type chosen based on the case.
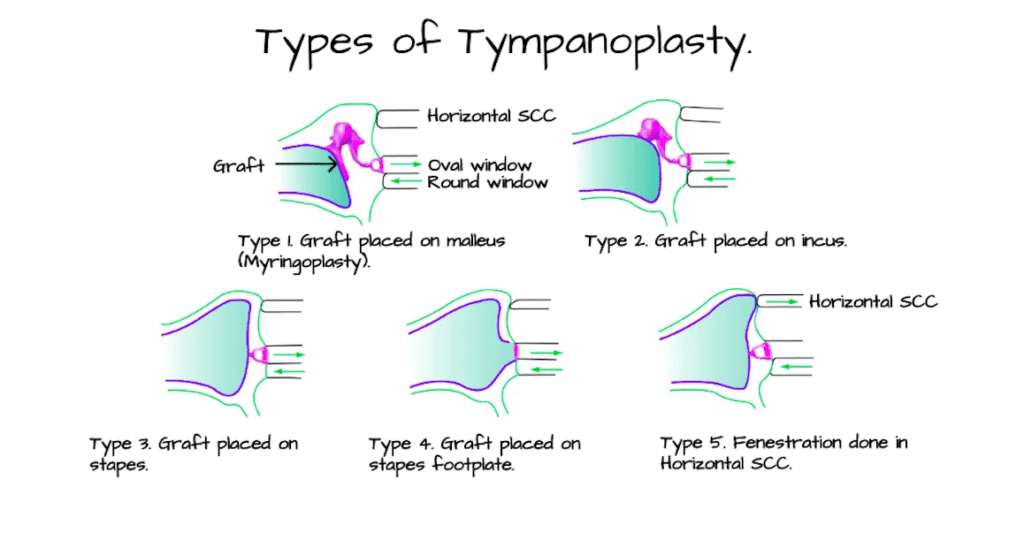
Ossicle Reconstruction
If the middle ear’s tiny bones are damaged, the surgeon may perform ossiculoplasty during tympanoplasty. This involves repairing or replacing ossicles with prosthetics. Research emphasizes its importance in hearing improvement surgery, particularly for otosclerosis or severe infections. It’s akin to rebuilding a pathway for sound to reach the inner ear effectively.
Tympanoplasty vs. Myringoplasty: What’s the Difference?
Tympanoplasty and myringoplasty both repair the eardrum but differ in scope. Myringoplasty focuses solely on patching an eardrum hole, often taking 30 to 90 minutes and sometimes using local anesthesia. Tympanoplasty addresses both the eardrum and middle ear issues, such as damaged ossicles or cholesteatoma, requiring general anesthesia and more recovery time.
Here’s a comparison:
- Myringoplasty: Repairs only the eardrum. Suited for small, central holes. Often done via the ear canal. Success rate around 94%.
- Tympanoplasty: Fixes the eardrum and middle ear structures. Used for complex cases like otosclerosis or adhesive otitis. May involve incisions. Success rate around 90%.
Research shows myringoplasty is common in children due to simple perforations from infections. Tympanoplasty is more typical for adults with chronic issues or trauma. Both aim to enhance hearing and prevent infections, with the choice depending on the damage’s complexity.
When Myringoplasty Is Preferred
Myringoplasty is ideal for straightforward eardrum holes without ossicle involvement. It’s less invasive, often performed in an office for adults. Children may require a hospital due to anesthesia needs. Medical sources note it’s best for small perforations without middle ear disease. Its faster recovery appeals to those with busy schedules.
Complex Cases Requiring Tympanoplasty
Tympanoplasty is suited for more complicated situations, like cholesteatoma or ossicle damage. It’s more extensive, as surgeons may need to reconstruct middle ear components. Patient experiences highlight its transformative impact on chronic hearing loss or infections. The additional surgical effort often leads to significant hearing improvements.
Recovery Timeline After Surgery
Recovery from tympanoplasty spans a few weeks to months. Patients typically go home the same day, though some stay overnight if experiencing dizziness or nausea. The first week brings mild ear pain, dizziness, or bloody drainage, which usually subsides quickly. Doctors advise keeping the ear dry and avoiding strenuous activities for at least two weeks.
By the second week, a follow-up checks the graft and removes stitches. Most patients resume work or school within one to two weeks, but complete healing may take six weeks to three months. Hearing improvement often develops gradually as the eardrum heals. Research and patient accounts stress that following medical advice leads to better outcomes.
First Week Post-Surgery
The initial days focus on rest. Patients may experience balance issues or ringing in the ear. Pain medications ease discomfort. Keeping the ear canal dry—no swimming or unprotected showers—is critical. Medical sources emphasize this early period ensures the graft adheres properly. Patients should avoid forceful sneezing or nose-blowing to prevent pressure changes.
Long-Term Healing Process
Full recovery means a healed eardrum and stable hearing, which can take up to three months, especially after complex middle ear surgery. Regular checkups monitor progress. Some patients report on forums that hearing improvements emerged only after a couple of months. Patience is essential, as the ear adjusts over time.
Possible Complications and Post-Surgery Guidelines
Tympanoplasty carries rare risks. The graft may fail to heal, leaving the hole open in about 5-10% of cases. Infections can occur, potentially leading to serious issues like meningitis. Other risks include facial muscle weakness, dizziness, or bleeding. Patients should contact their doctor immediately for high fever, severe pain, or heavy bleeding.
To minimize complications, patients should follow these guidelines:
- Keep the ear dry for at least six weeks.
- Avoid vigorous exercise or heavy lifting for two weeks.
- Sneeze with the mouth open to reduce ear pressure.
- Refrain from flying until cleared by the doctor.
- Use prescribed medications to prevent infection or manage pain.
Studies highlight that keeping the ear dry is critical for successful healing. Patients who disregard this advice often face issues like graft failure.
Managing Pain and Discomfort
Ear pain after surgery is common but manageable with medications like ibuprofen. Some patients experience dizziness, particularly if the middle ear was involved. Resting in a calm environment helps. Medical sources note that pain typically eases within a week. Persistent pain warrants a call to the ENT specialist.
Preventing Infections
Infections pose a significant risk after ear reconstruction. Doctors may prescribe antibiotics to prevent bacterial growth. Research indicates that patients who keep their ear dry and clean have fewer complications. One study noted higher infection rates when the ear gets wet prematurely. Simple precautions, like using a shower cap, can prevent setbacks.

Modern Techniques: Traditional vs. Flap Tympanoplasty
Tympanoplasty techniques have advanced over time. Traditional tympanoplasty uses a microscope and often involves an incision behind the ear. Surgeons patch the eardrum with tissue like temporalis fascia. It’s effective but can be invasive for complex cases. Studies report success rates around 90%.
Flap tympanoplasty, or endoscopic tympanoplasty, uses a small camera through the ear canal, avoiding external incisions. It’s less invasive, with faster recovery and minimal scarring. However, it’s less suitable for large perforations or ossicle repairs due to the ear canal’s limited space. Research shows comparable success rates but quicker healing for simpler cases.
Benefits of Endoscopic Methods
Endoscopic flap tympanoplasty is popular for its minimal invasiveness. No external incision means less pain and scarring. Patients on forums appreciate the quicker return to normal activities. However, it demands a skilled surgeon due to the ear canal’s constraints. It’s most effective for smaller perforations or when appearance is a concern.
Advantages of Traditional Methods
Traditional tympanoplasty excels in complex middle ear surgery. It offers better visibility for ossicle repairs or cholesteatoma removal. It’s widely used in hospitals with standard equipment. Research confirms it remains the preferred choice for challenging cases, despite longer recovery times.
FAQ: What Patients Often Ask About the Procedure
Patients frequently have questions about tympanoplasty, drawn from forums and medical sources. Here are common concerns:
Does hearing improve immediately?
Not always. Hearing after surgery may improve over weeks or months as the eardrum heals. Some patients notice significant changes; others see gradual progress.
Is the surgery painful?
Patients are under anesthesia during the procedure, feeling no pain. Post-surgery, mild ear pain or soreness lasts a few days, manageable with medication.
Can children undergo tympanoplasty?
Yes, but doctors typically wait until children are around 7 or 8 to follow recovery instructions. Myringoplasty is more common for younger patients.
What happens if the graft fails?
In 5-10% of cases, the graft doesn’t hold, leaving the hole open. Another surgery may be needed, but doctors first investigate the cause.
When can patients swim again?
Doctors advise waiting at least six weeks to keep the ear dry. Patients should consult their ENT before swimming.
These questions reflect common patient concerns, helping reduce anxiety about the procedure.
Tympanoplasty offers a reliable solution for repairing a perforated eardrum or damaged middle ear bones. It addresses chronic infections, hearing loss, or trauma, aiming to restore hearing and prevent ear issues. Whether it’s a simple myringoplasty or complex middle ear surgery, the procedure can significantly improve quality of life. Recovery requires patience, typically weeks to months, but most patients experience meaningful improvements. Following medical advice, especially keeping the ear dry, enhances success rates. This overview aims to demystify the process, helping patients feel informed and prepared.